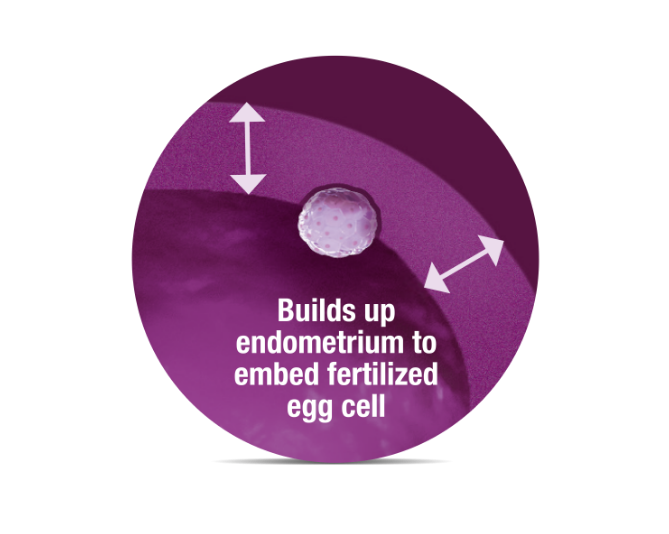
It is important that the uterine lining develops sufficiently to promote the successful implantation of the fertilised egg cell. In this context, the intake of PROFERTIL® female is recommended because this clinically tested product supports the implantation of the egg cell and can increase the chance of pregnancy.
The fertilised egg cell has already spent 4-6 days travelling down the fallopian tube before it reaches the uterus to implant. If the lining has already thickened in this period, it will be in an ideal state for the successful implantation of the egg cell. The implantation is called “nidation” in medical jargon.
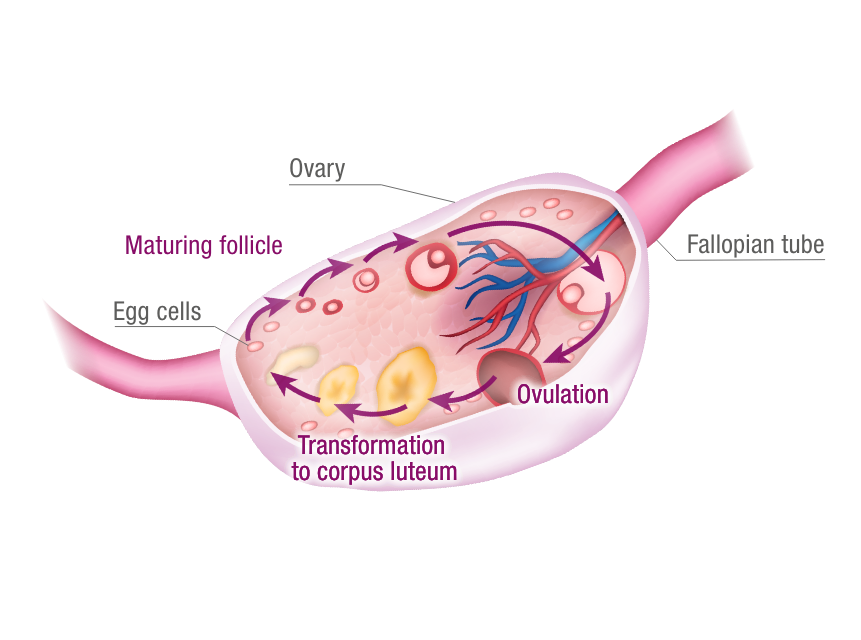
The period of the second half of the cycle is dominated by the luteal hormone progesterone and initiated with ovulation. The shedding of the uterine lining (endometrium) is prevented by progesterone in this period. If fertilisation does not occur, the corpus luteum dies. The female body simultaneously sheds the unnecessary uterine lining, i.e. part of the endometrium, in her monthly period.
The endometrium is normally located in the uterus. However, it can also grow outside, e.g. in the abdomen. If this is the case, it is referred to as endometriosis, which is a chronic disease. Above all, women with a polycystic ovary syndrome (PCOS) (disturbance in the hormonal cycle) have a higher probability of contracting it. Endometriosis increases the risk of infertility.
What is the two-layered uterine lining all about?
Studies have demonstrated that the chances of implantation improve when the lining has two layers in an ultrasound scan. Thus, an optimally built-up lining shows a three-line structure. These form the boundaries of the two lining layers to each other and the surroundings. The medical term for this is a trilaminar structure.
Unfavourable conditions for implantation
Insufficient thickness (less than 8-14 mm) and poor blood circulation to the lining are considered unfavourable conditions. PROFERTIL® female, a study-proven micronutrient combination, also provides the option of helping to develop the lining and thus improving endometrial receptivity without taking hormones.
For example, with regard to polycystic ovary syndrome, a hormonal imbalance often means that the normal development of the lining is not possible due to a lack of essential nutrients. It may be that the endometrium is too thin and also poorly supplied with blood in women with PCOS.
Which causes are responsible for a thin uterine lining?
Oestrogen deficiency as well as circulatory disorders and anaemia are at the forefront. It can also be caused by uterine fibroids, hydrosalpinx (at the ends of blocked fallopian tubes), endometritis (inflammation of the lining) as well as the scarring of the uterus. The same is true for an infection of the pelvic floor, the improper scraping of the uterus, long-term hormonal contraception and the intake of Clomiphene.
What treatment options are available?
The improvement of conditions for the implantation of the embryo is the top priority for developing the lining. For example, what can be done to improve the blood circulation of the endometrium? This can ultimately increase the chance of becoming pregnant.
PROFERTIL® female provides targeted and study-proven support for increasing the chance of a successful pregnancy.
Development of the uterine lining in the context of IVF treatment
In this context, appropriate hormones, such as progesterone, can be administered in connection with a diagnosed corpus luteum insufficiency. PROFERTIL® female can be taken in a supporting capacity, which is shown in the findings of the study at the Medical University Hospital of Vienna. This means that the chances of pregnancy increase.

The intake of vitamin D3
A woman’s cycle can be regulated with vitamin D3. This vitamin also helps with the maturation of egg cells and the development of the uterine lining so that the woman can become pregnant. However, it is essential to ensure that vitamin D3 is dosed and taken according to one’s own needs. This can be done very easily with vitamin D3 in droplet form. In order to precisely ascertain the need for vitamin D3, the vitamin status should be determined in advance in the laboratory.



